Dr Noor Alhashimi, Dr Yasmin De Alwis
Becoming a teenager is a big milestone in a young person’s life, as they take a step closer towards being an adult. In healthcare, this is also when young people transition from children’s health services to the adult services.
Essentially, everything and everyone they have become used to in their healthcare journey is about to change.
This is where transition services come in, aiming to help a young person move as smoothly as possible from a child centered to an adult centered healthcare system. It should be a gradual and planned process with the goal of providing healthcare that’s seamless, coordinated, and comprehensive.
As paediatricians, we’re ususally the ones who know the young person and their carers best, so it puts us in the best position to advocate for good transitional care.
But to understand what ‘good’ transition looks like, we need to first understand the barriers, so that we can build the bridges necessary to get the young person over to the adult side. And that’s what this article is all about.
Let’s look at some numbers
We’re getting better at treating children with long-term and life-limiting conditions, which means more are surviving into adulthood. A 2022 study found that there was a 68% rise in the number of young people reaching transition age in 2018/19 vs 6 years earlier).
This has massively increased the pressure on transition services. When the services can’tt keep up, the impacts are felt [KK1] in in the form of missed appointments, regular attendances to A&E, more frequent hospital admissions, unmet needs, and deterioration in health and quality of life.
There’s an even bigger challenge for young people with complex needs who are often left to find their way in a system with no clear pathway or designated adult transition lead.
Making the transition
There’s no ‘one size fits all’ for transition – Tthe timing for it can vary depending on the young person’s individual needs and current situation.
NICE guidelines recommend that the transition process should begin during a time of relative stability for the young person, and recommends starting at age 13- 14, or straight away for patients who have entered the service in later childhood, close to the point of transfer.
Early planning is important to give enough time to prepare for a successful transition. You can get a sense of this from the quotes of families involved (see below).
Barriers and Challenges
A survey by the Disabled Children’s Partnership gives some concerning insight into into the experience some disabled young people (16+) and their families have had with transitional services.
- 56% of families in the survey did not have a transitional plan in place.
- 75% of families faced challenges with healthcare transitions
These aren’t just statistics. They’re a reflection of the stress and uncertainty that many families face during healthcare transitions.
Here are some quotes from parents
“During childhood, the paediatrician pulls all the services together but there is no equivalent when my child moved across to adult service. No one clinician other than the GP.”
“As a parent I thought that transition was meant to start at the age of 16, however my daughter turned 18 last August and we have had one transition meeting. Not any more meetings since the first one when she was 16”.
A research study in Wales found common themes that were barriers to a successful transition, echoing the concerns of these parents.
- Delay in identifying that the young person needed transition to adult services, and lack of preparation for the family
- Poor communication and lack of collaboration between the services involved.
This is where having an identified key worker to coordinate the transition is helpful A a joint assessment, involving key professionals is best practice, so that a single transition plan is made that meets the needs of the young person.
3. Children’s Services and Adult Services function differently
Children’s services – look at the child in the wider context of the family. It’s more likely to take a ‘family centered’ approach.
Adult services – focus more on the individual and the individual’s specific needs.
This can come as a ‘culture shock’ to families.
4. Changes in support threshold
Adult services might have different thresholds to offer certain levels of support, such social support, to the young person and their family, which could mean the young person’s situation needs to get worse before it’s acted upon.
Money Money Money… at the moment, transitional care is funded by children’s services. The problem here is thattransition doesn’t stop with handover – it usually continues until a young person is in their twenties. This means that adult teams have fewer resources and less time to focus on transition. If both services were to contribute financially, then transition would become more of a shared responsibility and a real priority.
What does good transition look like for children with complex needs?
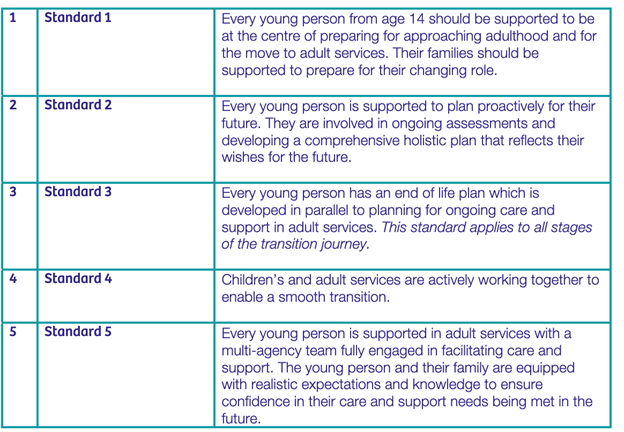
Together For Short Lives gives 5 key standards for agood transition.
As you can see, there’s a lot that goes into providing ‘good transition services’, and it all starts with our training.
Including transitional care into job plans, making training mandatory, and and giving staff protected time to work on a growing service is key to building an effective service. (You can’t work on something if you don’t have the time for it!)
As well as these key standards, ‘Hospital passports’ for children with additional needs, like the one used at the Great North Children’s Hospital in Newcastle, can help make for an easier transition, so long as the information in them is comprehensive and regularly updated. The passport helps give a snapshot of who the young person is, their likes and dislikes, medical background, support system, and the professionals and teams involved in their care.
Summary
Transitioning from paediatrics to adult care is a challenge for us, and for our patients. Even more so for young people with complex needs who are at higher risk of getting ‘lost’ in the system.
Transition has a big impact on the life and health of patients, so it should be a shared responsibility that spans across services and systems, and should not fall on the shoulders of one team or clinician. .
Key Points
- 1. Start the process early
- 2. Understanding the barriers to good transition can help make sure young people aren’t disadvantaged by the process
- 2. The 3 C’s – Communicate, Collaborate, and Campaign.
- Communicate with young people and their families to understand what they needCollaborate across services to deliver coordinated and uninterrupted care. This also includes education, social care, and primary care. Remember, your GP is the only clinician that doesn’t change as you grow older!
- Campaign for ways to improve the system, so that patients and their families benefit from better outcomes and experiences
Authors
Dr Noor Alhashimi ST4 Paediatrics, North East of England Deanery
Expert Reviewer: Dr Yasmin De Alwis, Consultant Neurodisability Paediatrician, Great North Children’s Hospital Newcastle Upon Tyne.
