Dr Jonathan Round – PICU Consultant
When I left my first spell in neonatal training, I thought there were just two inotropes – dopamine and dobutamine. There was a myth of another agent called adrenaline and the even more elusive noradrenaline, but no one seemed to survive after these drugs. Later, in ICU training, I came across strange agents that I could not even spell, before working out the simple and the basic principles that have helped me and my patients ever since. Fundamentally, inotropes are properly dangerous drugs, and should only be used if you and the rest of the team know what they are doing, and the patient is properly monitored.
The key to proper use of inotropes is to first understand what each drug does, then to choose those that fit the clinical problem your patient has, and lastly to set up monitoring for the patient so they get the right amount of the right agent.
So what do they do??
Inotropes make the heart beat more forcefully. Not all agents in the group we are looking at here do that much – Vp and Na have minimal inotropic action at all. Inotropes work by increasing the cycling of calcium in and out of cardiac muscle. They either work by Beta-adrenergic stimulation (Da, Db, Adr) or phosphodiesterase 3 inhibition (milrinone). Both mechanisms increase intracellular cAMP.
Common Agents
- Dopamine (Da)
- Dobutamine (Db)
- Adrenaline (Adr)
- Noradrenaline (Na)
- Vasopressin (Vp)
- Milrinone (Mi)
Chronotropes work by making the heart beat faster, primarily by Beta-adrenergic stimulation (Da, Db, Adr).
Vasoconstrictors are helpful to raise the blood pressure by increasing peripheral vascular resistance, but at the expense of making the heart work harder. This is primarily through Alpha – adrenergic activation (Na, Adr, Da at higher dose (allegedly)), or vasopressin receptors (Vp).
Vasodilators reduce peripheral vascular resistance. This can ease the work of the heart and improve features of heart failure, but it may lead to a lower blood pressure. Agents work by reducing intracellular calcium in the muscle of the blood vessels either by Beta-adrenergic stimulation (Db, Da low dose (allegedly)), or via cAMP (Mi).
Redefining the problem
Inotropes, or cardiovascularly active agents, can be used in two main scenarios which often overlap. Understanding the basics of how the heart and the CVS works is essential to picking the right agents.
#1 Cardiac output too low to meet the needs of the body
#2 Blood pressure too low to perfuse all the capillary beds.
It is essential that #1 is looked for and addressed before #2 is managed.
#1 Low Cardiac Output
Cardiac output is the product of heart rate and stroke volume. Heart rate is easy to count, but stroke volume harder to measure, even indirectly. It is related to all of the filling pressure (preload), contractility of the heart and the force resisting the heart pumping (afterload, and nearly the same as the blood pressure).
Low cardiac output state may manifest as a pale patient, prolonged central refill, low GCS, high lactate or low central venous saturations. There are adjuncts to the measurement of stroke volume, including echocardiography, indirect calorimetry, oesophageal Doppler and pulse wave contour analysis. All are more useful to follow trends rather than make absolute measurements.
The strategy for managing low cardiac output is as follows:
- Optimise preload
- Optimise heart rate
- Improve contractility
[and also set up suitable monitoring]
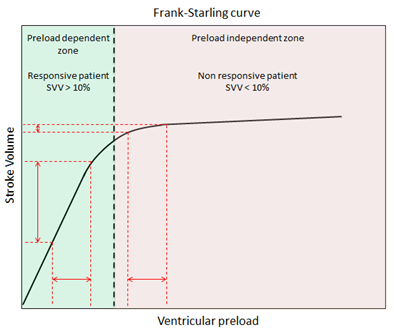
Preload is improved with fluid. This can be done with monitoring, raising the CVP to 8-10 mmHg, or by guesswork. Here fluid is given rapidly, partly to correct a low preload state, and partly to see where the heart is on the Starling curve. [and Starling raises its head at last].
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Starling in three sentences
+ Starling got the recognition for work done also by Frank and Maestrini.
+ The ‘law’ states that as ventricular diastolic volume or right atrial pressure increases, so does the force of contraction or stroke volume.
+ This relationship breaks down when the ventricle reaches a certain size, and force of contraction or stroke volume can no longer increase.
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
The key is to give the fluid fast and give enough. 20 ml/kg over 20 mins unless in possible heart failure. If the BP and HR improve, it was fluid responsive and you are on the steep bit of the curve. More fluid may help more.
However if it did little, the situation is fluid unresponsive and you are on the flat bit of the curve. This has several implications:
Implications of Fluid Unresponsive Low Cardiac output state:
- the CVS is dysfunctional in itself
- the patient is decompensated and may die without intervention
- a central line is needed
- augmented monitoring is needed. (CVP, lactate, MVSaO2, arterial line)
Having optimized preload, next is optimizing heart rate. The ideal is the rate that the child would have during moderate exercise. Higher than this, there is insufficient time to fill the ventricles and stroke volume will suffer. Less and there are not enough strokes to pump the blood. As a guide this will be 160-175/min for the neonate; 125-145 for a 5 year old; 110-130 for a teenager.
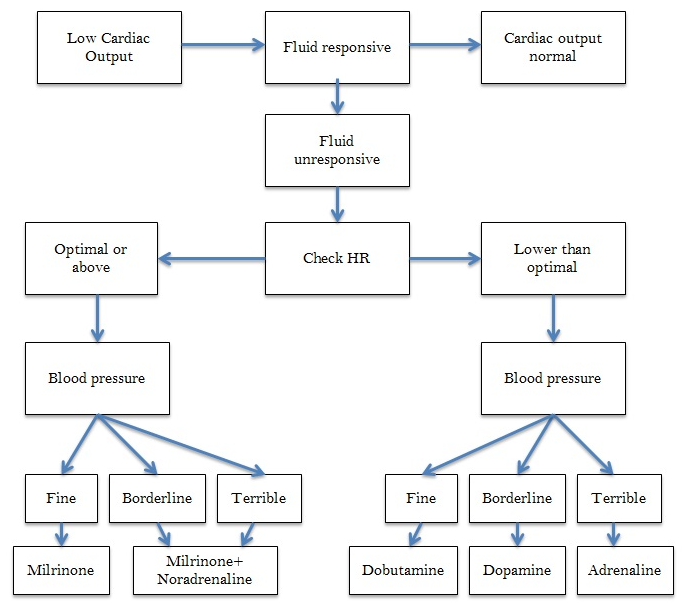
Mostly the drugs we use to alter rate have another action, so will affect cardiac output blood pressure too. Adr is also improves contractility and vasoconstricts; Db gently improves contractility and vasodilates, Da also gently improves contractility and vasoconstricts at higher doses. So choice of agent depends on other factors, particularly the blood pressure. This is my mental algorithm:
The agents used to speed up the heart also improve contractility. However, what if the heart is already beating at a suitable rate, or even faster than you want? Here the best thing is to choose an agent that will improve contractility but not raise the heart rate. That agent is milrinone. Its place in the algorithm is shown above. Although a useful inotrope, its other effect is as a vasodilator. So if there is an issue with the blood pressure being lowish, it will get lower with the milrinone. Hence a vasoconstrictor can be used alongside the milrinone, and Noradrenaline is a good choice. This can be titrated against the BP.
#2 Blood pressure too low
Often, when the cardiac output is addressed properly, as above, the blood pressure is not an issue. However there are some situations where this is not the case – the cardiac output is normal or above, but the BP is too low. These are the typical characteristics of such a child:
- HR raised
- CRT brisk
- Liver normal size
- CVP low/normal
- Lactate normal (usually)
- Pulse bounding/high volume/wide pulse pressure
- Appearance Flushed
- Fluid response Brief
Physiology
The commonest cause for this scenario is cytokine-driven vasodilation. Here the low vascular tone prevents the cardiac output making an adequate blood pressure. CVS reflexes lead to tachycardia. Fluid may boost the cardiac output, but with nothing to pump against, the BP rises transiently only. As cardiac output is good, usually cellular oxygen supply is adequate and the lactate is normal. [however, if the low BP prevents all capillary beds being perfused or there is a tissue dysoxia, lactate may rise].
Management
The treatment here is primarily with vasoconstrictors. Noradrenaline is first choice, and titrated to the desired BP. When using this, be aware that increasing the vascular tone may put extra strain on the heart and it may begin to fail, leading to a low cardiac output. Additional agents such as milrinone or adrenaline may be needed.
Summary
- Understand what is wrong with the patient physiological
- Choose interventions that address this.
- Choose monitoring to better explore the CVS.
- Remember that the situation may change – a new physiological scenario may emerge.
Dr Jonathan Round, PICU Consultant

I would argue that Dopamine has fallen out of favor in many ED and Critical Care settings – Epinephrine (Adrenaline across the pond) would be used its the first pressor for fluid refractory shock in low BP states. it can be safely given through a peripheral IV and IO as well.
i’d agree with you Brad – it isn’t quite this, but DA functions like weak adrenaline.
Pingback: Don’t Panic! The PICU starter pack is here…
Great article, wish i had this prior to doing my first PICU placement!! Definitely would have made things easier to understand.
Awesome, Genius!. I appreciate your contribution. I was taking PALS……..
Good snapshot knowledge of inotropes! Enjoyed reading it! Thanks!
Great document which has been pushed out to me as a student nurse!
Great breakdown. I am reading to make a simple presentation for interns & this is very useful to simplify things for myself & them.
Thanks for your feedback!